Pinning down malevolent cancer cells
A breast cancer diagnosis is, of course, bad news. But prognosis can be good if the tumor hasn’t yet released cellular scouts into the bloodstream. Known as circulating tumor cells, or CTC’s, the cells break away from primary tumors and migrate through the blood to colonize new territory.
Once cancer has metastasized to a new site, the disease is much harder to treat. If as few as five CTC’s are detected among a billion normal cells in a typical-sized blood draw, prognosis plummets, says UC Berkeley’s Lydia Sohn, but the threatening cells remain poorly understood, stalling efforts to block metastasis.
Researchers know there are different types of CTC’s, distinguished by different combinations of proteins arrayed on their surfaces. The proteins identify the state of the cell, and some play key roles in communication between cells. But without knowing how many CTC types there are, or if different ones pose different risks, countering CTC’s malevolent mission remains out of reach.
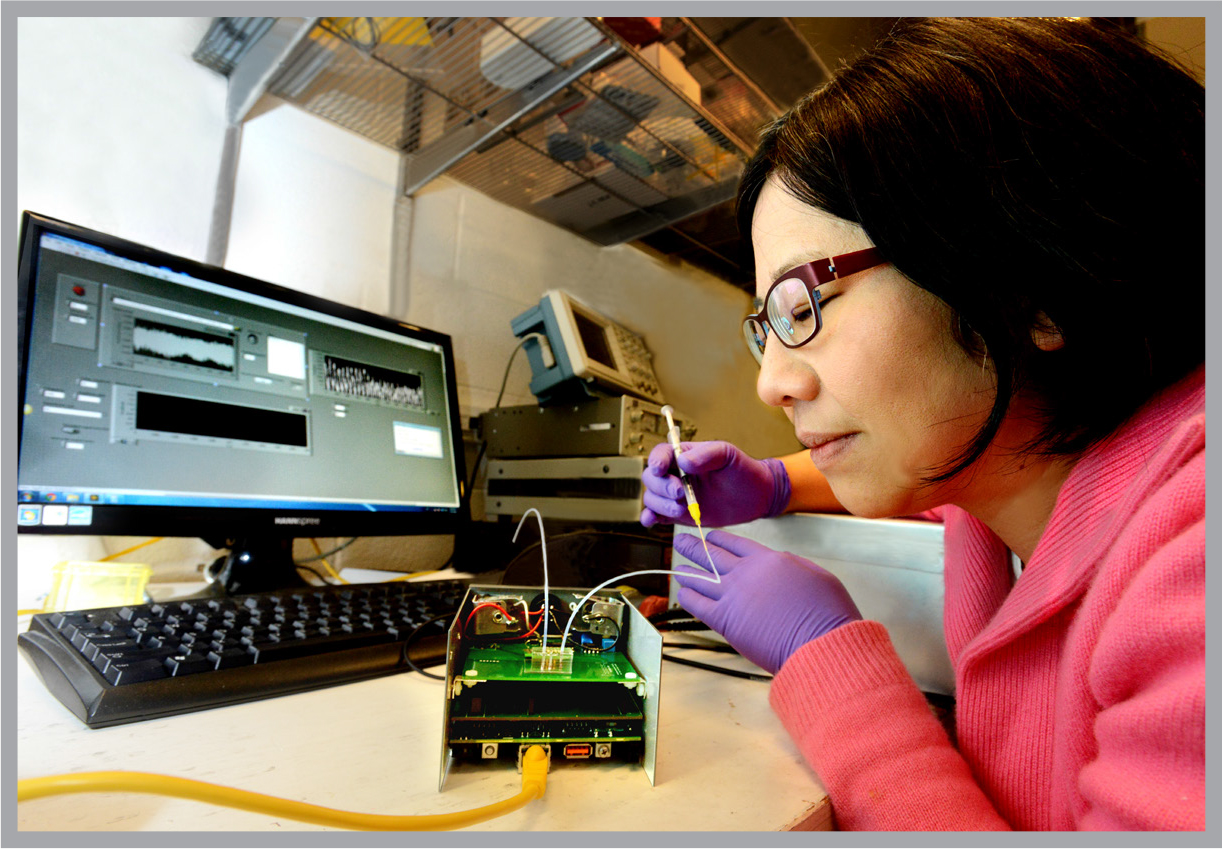
With support from the Bakar Fellows Program, Sohn and her lab are developing a new technique based on microtechnology to distinguish between different types of CTC’s. The strategy identifies the cells without interacting with them as conventional biological tagging does, eliminating the risk that the very act of studying the cells will change their character.
She hopes the more sensitive approach will help clinicians learn which CTC’s are most prone to lead to metastasis. The specific CTC’s, identified by their surface proteins, could then become targets for new drugs to disable them or block their advance.
“For me, it’s a chance to see an immediate effect – at least I want to believe it. No one should have to suffer through these kinds of cancer.”
An associate professor mechanical engineering, Sohn aims to demonstrate benefits of applying the technology known as microfluidics to pin down CTC suspects.
The process works somewhat like a pinball game. Blood from metastatic breast cancer patients is pumped through microchannels less than a thousandth of an inch in diameter, imbedded in a transparent plastic chip. Sohn pre-coats different sections of the channel with different antibodies – each able to interact with only one type of surface protein.
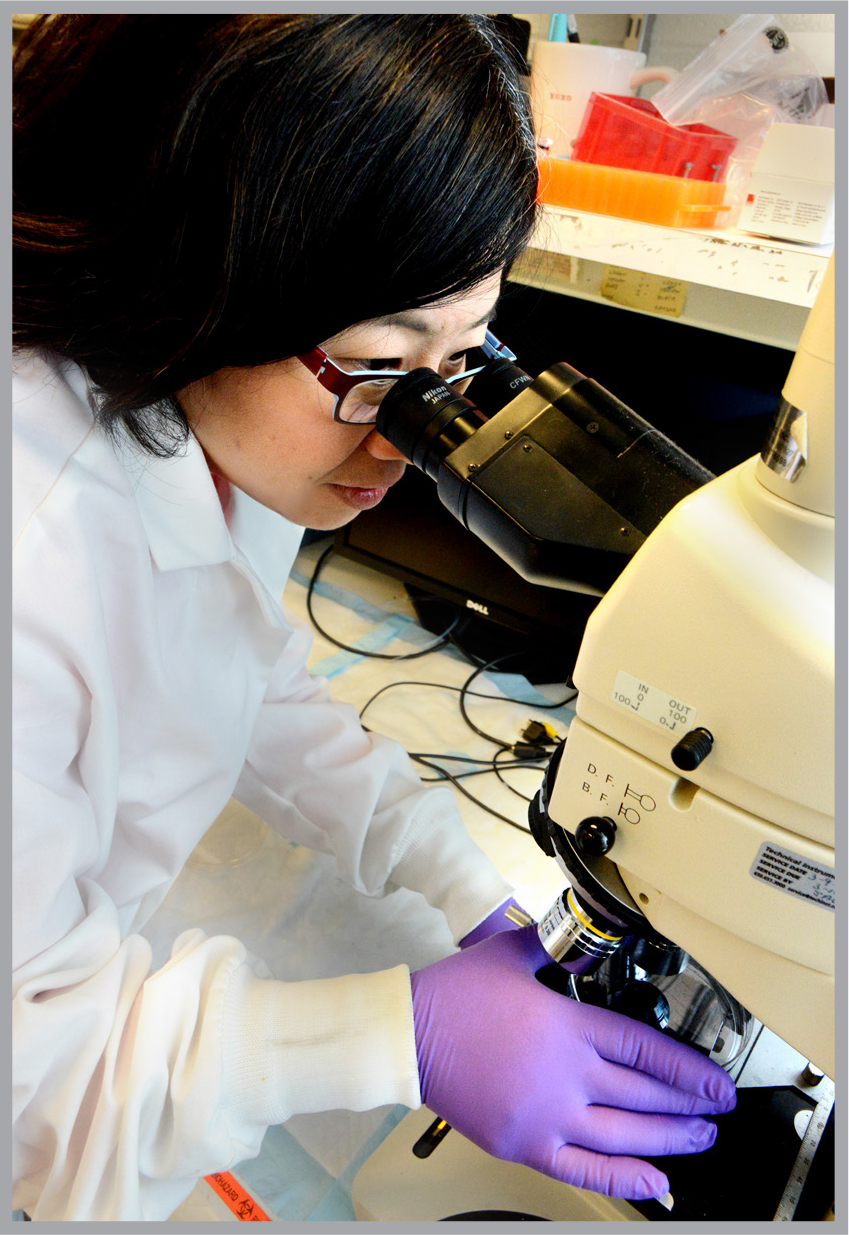
As a cell in the blood flows through the channels, its progress slows whenever one of its surface proteins encounters its matching antibody. By recording precisely where in the channel the cell’s momentum slows, Sohn can identify which proteins are on its surface.
With the microchannels, Sohn can look for a whole panel of protein biomarkers without risk of interfering with the cells.
“The Bakar funding has got us off to a very good start,” she says. “The kind of research I do is ‘out there’ – unconventional. Once we’ve established the sensitivity of our microfluidics approach, we can seek more traditional funding and transition it into clinical use.”
A clinical application of microfluidics is a long way from where Sohn started in the field. Her PhD and postdoctoral research were in physics, focusing on superconductivity. She turned to biomedical applications because “I thought there were more interesting problems – more unknowns. How do you uncover all the parameters that control a cell? How do you capture single cells?”
Recently, studies have begun to show that some CTC’s develop stem cell qualities.
“The current hypothesis is that these cells that may be responsible for metastatic tumors,” Sohn says. She aims to use the microfluidics device to study these cells too – to determine how often they are present at different stages of cancer, and under what conditions CTC’s express these stem cell-like traits.
Sohn’s lab is also collaborating with Haiyan Huang, an associate professor of biostatistics at Berkeley, to tease out the clusters of genes linked to different cancer cell activities.
Sohn’s basic microfluidics strategy can also be applied to diagnosing different types of cancer. And because it is simpler and cheaper than more conventional approaches, it may find use where more expensive technology is beyond reach.
“There is a drastic difference in cure rates for childhood leukemia in industrial versus non-industrial countries,” she says.In the U.S. and Europe, about 80 percent of kids with leukemia are cured. But in less developed countries the cure rate is less than 10 percent. “The major reason for this is that expensive, complex medical devices are less available, and so the disease often goes undetected or misdiagnosed.”
Meanwhile, the Sohn lab is already seeking collaborations with clinicians to use her biomarker technology to identify different types of CTC’s in patients.
“We’re definitely hoping to make inroads. We want to make a difference,” she says.
____________________________
The Bakar Fellows Program supports innovative research by early career faculty at UC Berkeley with a special focus on projects that hold commercial promise. For more information, see http://bakarfellows.berkeley.edu.
