New Research Finds Deep-Sleep Brain Waves Predict Blood Sugar Control

Illustration by Neil Freese, photography courtesy Aaker, isens usa / Unsplash
Researchers have known that a lack of quality sleep can increase a person’s risk of diabetes. What has remained a mystery, however, is why.
Now, new findings from a team of sleep scientists at the University of California, Berkeley, are closer to an answer. The researchers have uncovered a potential mechanism in humans that explains how and why deep-sleep brain waves at night are able to regulate the body’s sensitivity to insulin, which in turn improves blood sugar control the next day.
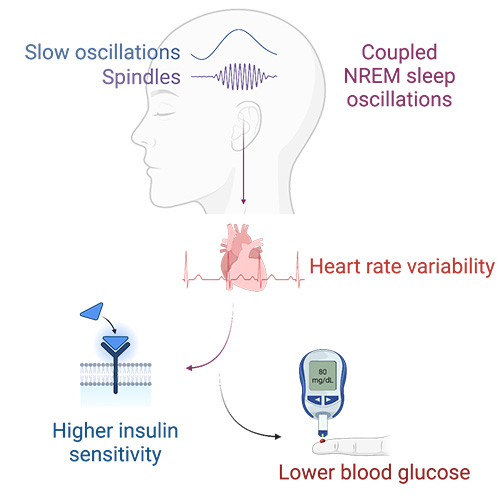
“These synchronized brain waves act like a finger that flicks the first domino to start an associated chain reaction from the brain, down to the heart, and then out to alter the body’s regulation of blood sugar,” said Matthew Walker, a UC Berkeley professor of neuroscience and psychology and senior author of the new study. “In particular, the combination of two brain waves, called sleep spindles and slow waves, predict an increase in the body’s sensitivity to the hormone called insulin, which consequentially and beneficially lowers blood glucose levels.”
The researchers say this is an exciting advance because sleep is a modifiable lifestyle factor that could now be used as part of a therapeutic and painless adjunct treatment for those with high blood sugar or Type 2 diabetes.
Scientists also noted an additional benefit besides the potential new mechanistic pathway.
“Beyond revealing a new mechanism, our results also show that these deep-sleep brain waves could be used as a sensitive marker of someone’s next-day blood sugar levels, more so than traditional sleep metrics,” said Vyoma D. Shah, a researcher at Walker’s Center for Human Sleep Science and co-author of the study. “Adding to the therapeutic relevance of this new discovery, the findings also suggest a novel, non-invasive tool — deep-sleep brain waves — for mapping and predicting someone’s blood sugar control.”
The team’s findings were published today in the journal Cell Reports Medicine.
For years, researchers have studied how the coupling of non-rapid eye movement sleep spindles and deep, slow brain waves corresponded to an entirely different function — that of learning and memory. Indeed, the same team of UC Berkeley researchers previously found that deep-sleep brain waves improved the ability of the hippocampus — the part of the brain associated with learning — to retain information.
Matthew Walker
But this new research builds on a 2021 rodent study and reveals a novel and previously unrecognized role for these combined brain waves in humans when it comes to the critical bodily function of blood sugar management.
The UC Berkeley researchers first examined sleep data in a group of 600 individuals. They found that this particular coupled set of deep-sleep brain waves predicted next-day glucose control, even after controlling for other factors such as age, gender and the duration and quality of sleep.
“This particular coupling of deep-sleep brain waves was more predictive of glucose than an individual’s sleep duration or sleep efficiency,” said Raphael Vallat, a UC Berkeley postdoctoral fellow and co-author of the study. “That indicates there is something uniquely special about the electrophysiological quality and coordinated ballet of these brain oscillations during deep sleep.”
Next, the team then set out to explore the descending pathway that might explain the connection between these deep-sleep brain waves sending a signal down into the body, ultimately predicting the regulation of blood glucose.
The findings from the team reveal an unfolding set of steps that could help explain how and why these deep-sleep brain waves are related to superior blood sugar control. First, they found that stronger and more frequent coupling of the deep-sleep brain waves predicted a switch in the body’s nervous system state into the more quiescent and calming branch, called the parasympathetic nervous system. They measured that change in the body and the shift to this low-stress state using heart rate variability as a proxy.
Next, the team turned its attention to the final step of blood sugar balance.
The researchers further discovered that this deep sleep switch to the calming branch of the nervous system further predicted an increased sensitivity of the body to the glucose-regulating hormone called insulin, which instructs cells to absorb glucose from the bloodstream, preventing a deleterious blood sugar spike.
That’s particularly important for people trying to back away from hyperglycemia and Type 2 diabetes.
“In the electrical static of sleep at night, there is a series of connected associations, such that deep-sleep brain waves telegraph a recalibration and calming of your nervous system the following day,” Walker said. “This rather marvelous associated soothing effect on your nervous system is then associated with a reboot of your body’s sensitivity to insulin, resulting in a more effective control of blood sugar the next day.”
The researchers subsequently replicated the same effects by examining a separate group of 1,900 participants.
“Once we replicated the findings in a different cohort, I think we actually started to feel more confident in the results ourselves,” Walker said. “But I’ll wait for others to replicate it before I truly start believing, such is my British skepticism.”
The scientists said the research is particularly exciting given the potential clinical significance years down the line. Diabetes treatments already on the market can sometimes be difficult for patients to adhere to. The same is true of the recommended lifestyle changes, including different eating habits and regular exercise.
Sleep, however, is a largely painless experience for most people.
And while sleep is not going to be the single magic bullet, the prospect of new technologies that can safely alter brain waves during deep sleep that this new research has uncovered may help people better manage their blood sugar. That, the research team said, is reason for hope.
