
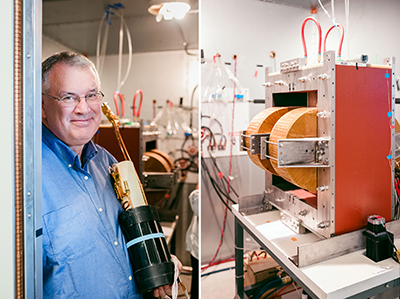
Steven Conolly
BioengineeringElectrical Engineering and Computer SciencesSteven Conolly holds the Montford G. Cook Chair in the College of Engineering, where he is Professor of Bioengineering, and Electrical Engineering and Computer Sciences. He is a medical imaging innovator, with particular emphasis on Magnetic Particle Imaging. He received his B.S in Electrical Engineering from Boston University, and his M.S. and Ph.D. in Electrical Engineering from Stanford University.
Steven Conolly was a 2022 Bakar Prize recipient.
Bakar Prize Project
- Transfer the superferromagnetic (SFMIO) technology and synthesis to our startup company, Magnetic Insight.
- Excite two major campus collaborators (Phil Messersmith of MSE & BioE, Greg Tikhomirov of EECS) to apply their nanoparticle synthesis skills to synthesizing safe SFMIO tracers for in vivo applications.
- We started up a collaboration with CAR-T and CAR-NK cell immunotherapy experts Carl June (Penn) and more recently Michel DuPage at Cal.
- We published three key journal publications on SFMIO behavior and several conference abstracts and review articles.
- Three PhD students (Barry Fung, Caylin Colson, and Chinmoy Saayujya) published experiments that confirmed our nano-scale physics model, which prescribes chaining SPIOs as necessary and sufficient for SFMIO behavior. This crucial physics model will continue to inform our chemical synthesis.
Spark Award Project
MPI Tracers for Quantitative, High-Resolution Tracking of Advanced Cancer Immunotherapies without Radiation
Many of today’s most advanced diagnostic and therapeutic methods rely on injected cells, such as stem cells and modified immune cells. For example, the most exciting breakthroughs in oncology are in the field of immunotherapy, where the patient’s own white blood cells are engineered to better recognize and kill tumors. Development of these therapies has been slowed because it is extremely challenging to track injected cells within the body. Currently available nuclear medicine imaging methods; scintigraphy, PET, or SPECT, require radioactive reporters which can alter the viability of the cells under study. The Conolly laboratory is developing a high-resolution three-dimensional imaging method, Magnetic Particle Imaging, which does not use any radiation and has unprecedented sensitivity. Conolly’s Bakar Fellows project is to develop a high-resolution, safe and biocompatible tracer to enable MPI-based single-cell detection for immunotherapy optimization. This high-resolution tracer will also be useful for tracking stem cell therapies, and could potentially revolutionize diagnosis of pulmonary embolisms, stroke, and gastro-intestinal bleeds. This research may eventually compete for a significant fraction of the global contrast agent market, which now totals $4.57 billion annually.
Steven Conolly’s Story
It’s still some years off, but Steven Conolly aims to see disease in a totally new way. He leads research on an emerging imaging technology that already can peer past tissue or organs to detect disease deep within the body.
revolutionize early-stage diagnosis of diseases like cancer, stroke, gastrointestinal bleeds, or pulmonary embolisms.
Photo credit: Mark Joseph Hanson
Fibrous tissue can sometimes obscure an X-ray mammogram from detecting breast tumors. X-rays, of course, expose patients to radiation, as does more powerful PET scan imaging.
A new imaging technology, known as Magnetic Particle Imaging (MPI), uses neither radiation nor radioactive tracers. Under development for about ten years, MPI has already yielded high-quality scans in animal research.
The imaging system uses minute quantities of magnetic iron oxide “nanoparticles” as tracers – as little as two billionths of a gram. These are essentially flecks of rust, less than a thousandth the width of a human hair, and can be injected safely into a vein.
When delivered with precision, the nanoparticles can zero in on a disease target under scrutiny. The tracers show bright against a dark background and the intervening tissue is essentially invisible.
“It’s like looking for stars at night instead of during the day,” says Conolly, a professor of bioengineering and also electrical engineering and computer sciences.
“MPI can see the magnetic tracers with superb contrast and the physician can ‘see’ disease through the healthy background tissue.”
Getting the nanoparticles to specifically target disease is a key challenge to advancing MPI. With support from the Bakar Fellowship Program, Conolly’s team is developing techniques to allow the nanoparticles to congregate in tumors and other diseases with high specificity and resolution.
MPI is similar in some ways to MRI, but its novelty lies in the use of the magnetic nanoparticles. Exposed in succession to two magnetic fields, the particles “flip” north to south and then back again, much like water molecules do in an MRI exam. And as in an MRI, the energy released by this response is converted into voltage waveforms that can then be reconstructed into a detailed 3D image on a computer.
But where an MRI forms a picture of the water in the body, including muscles and tissue, MPI does not. It creates images only of the magnetic tracers.

Photo credit: Mark Joseph Hanson
When the MPI scans detect suspect diseased tissue, they can be overlaid on X-ray, CT or MRI “anatomic” images to show where the disease is in relation to anatomy.
Recent animal studies in collaboration with surgeon Jon Carter at UCSF and Seattle-based LodeSpin lab have shown that MPI can quickly pick up nanoparticles injected into a vein in order to detect life-threatening gastrointestinal bleeds.
Gut bleeds are currently diagnosed by nuclear medicine, but the procedure can be slow and exposes patients to radiation. The MPI image can get results in a few minutes with no obscuring background tissue and with no radiation dose.
“Safe and really rapid diagnosis of gut bleeds could definitely save lives.” Conolly says.
In collaboration with UCSF pulmonologist Payam Nahid, Conolly’s graduate students, Xinyi Zhou and Zhi Wei Tay, demonstrated that 3D MPI can safely provide the types of lung images needed to diagnose pulmonary embolism – rapidly and without radiation.
The lab has also shown that MPI can visualize cerebral blood volume, even in small capillaries — a potential new, high-contrast strategy to provide noninvasive diagnosis of stroke.
In another project, Conolly’s team is labeling immune cells with nanoparticles to detect early-stage lung cancer. The research team has already shown that MPI can noninvasively discern as few as 200 labeled cells in rats’ lungs — superior to other imaging methods.
The lab aims to improve scanner hardware and modify the magnetic nanoparticles to approach single-cell sensitivity for preclinical research studies – and one day a radiation-free complement to nuclear medicine diagnostic imaging.
“Our next challenge is to improve the nanoparticles for high-resolution images,” Conolly says. “That would translate into smaller, affordable scanners for diagnosing tumors and other diseases in patients.”
“I’m confident that research in our field will soon allow MPI to provide life-saving diagnoses and treatments.”